Report Published May 28, 2015 · Updated May 27, 2015 · 20 minute read
A Lifetime Electronic Health Record for Every American
David Kendall & Elizabeth Quill

Tracie Storie, a 52 year-old with a penchant for traveling, had come down with chills after a trip abroad where she had been suffering from a urinary tract infection.1 She was staying with her daughter in Boston over the weekend and was planning to return home to Austin, Texas. Her daughter insisted on taking to her to the emergency room because she couldn’t talk without her teeth chattering. The doctors discovered she had sepsis, a potentially fatal infection in the blood stream, which may have started with the urinary tract infection. But they couldn’t treat her. Tracie was allergic to certain antibiotics but was in no condition to recall the names of those drugs, and her medical records were locked up in her doctor’s office in Austin. On Monday, the doctors in Boston finally got her records from Austin. Tracie recovered, but she had to return to the ER a few days later with severe pain in her head and neck, which likely occurred due to the untreated sepsis.
Tracie would have suffered less and recovered more quickly if her medical records had been available digitally and under her control. Her brush with death occurred six years after President George W. Bush set a national goal for all Americans to have an electronic health record by 2014. Incredibly, despite this commitment and $30 billion in federal funding, neither Tracie nor hardly any other patient in America has a complete electronic record. Instead, while more records than ever are stored in the computer systems of individual hospitals and doctors’ offices, no one has the clear responsibility for assembling all the information about each patient in a complete package and making it available when needed. Providing all Americans with a complete, lifetime health record—compiled from individual systems and available 24/7—would improve the patient experience and ensure that patients get optimal care whenever and wherever they need it. And it would save the federal government $41.7 billion over ten years by eliminating wasteful, unnecessary care.
This idea brief is one of a series of Third Way proposals that cuts waste in health care by removing obstacles to quality patient care. This approach directly improves the patient experience—when patients stay healthy, or get better quicker, they need less care. Our proposals come from innovative ideas pioneered by health care professionals and organizations, and show how to scale successful pilots from red and blue states. Together, they make cutting waste a policy agenda instead of a mere slogan.
What is Stopping Patients from Getting Quality Care?
After more than a decade of efforts, no one in the country has a complete and comprehensive electronic health record (EHR). Instead, individual health information is stored in various places, and as records become increasingly digitized, they are seldom integrated. As of 2013, 39% of physicians reported electronically sharing data with other providers, however only 14% shared data with providers or hospitals outside of their organization.2
In 2009, Congress passed the Health Information Technology for Economic and Clinical Health Act (HITECH Act).3 Under this, the Department of Health and Human Services (HHS) was authorized to spend nearly $30 billion in Medicare and Medicaid incentive payments to expand the adoption of health information technology (HIT).4 When HITECH passed, policymakers imagined individual medical information being easily available to providers and patients. The hope was that this would facilitate coordinated care, avoiding medical errors and adverse reactions, and increase the overall quality of patient care while preventing redundancy.5
In order for providers to receive a portion of this $30 billion, HITECH requires “meaningful use” of EHRs.6 Meaningful use is a set of standards set by the Centers for Medicare & Medicaid Services (CMS) that includes various objectives, from maintaining active medications lists to electronic submission of lab tests.7 HITECH originally intended to gradually increase the meaningful use standards in order for medical professionals to receive the incentive payments. For Stage 2 meaningful use, the Office of the National Coordinator for Health Information Technology (ONC) has emphasized the sharing of health information between providers in an effort to improve care coordination. The goal of the sharing initiative is to move patient medical information to different providers who are using different information systems while maintaining the accuracy of the information transferred.
Adoption of EHRs has expanded rapidly. In 2013, 58.9% of U.S. hospitals had at least a minimum basic EHR8 and 78.4% of physicians used an EHR.9 However, the majority of these systems cannot exchange patient health information electronically. With over 550 certified medical information software companies in the United States selling over 1,100 programs,10 it is no surprise that these programs generally do not communicate with one another.11
This problem is called ‘lack of interoperability’, which simply means that one EHR system cannot readily exchange data with another system and interpret shared data.12 Interoperability requires agreement among competing EHR software companies on complicated, highly technical standards. In fact, through the leadership of Rep. Mike Burgess (R-TX), the House Energy and Commerce has included in its 21st Century Cures legislation a requirement that EHR vendors provide an interface for their software that would allow the patient records from other EHR systems to work in each other’s systems.13 But one simple requirement for interoperability is that each EHR system must know where to find the data about a patient that exists in other systems. A health information exchange provides the link in one of two ways. Some exchanges create an index of patients’ data that exists on each EHR system just as a phone book is an index of how to call people. That model is called decentralized because all the data stays on each EHR system and gets transferred using the index. The other model is centralized because it stores a copy of a patient’s data and sends the copy to an EHR system that can receive data from multiple sources just as every email software program can receive email for every other software program.
The HITECH Act also provided about $550 million for the development of health information exchanges in each state. Unlike the success of HITECH in getting health care providers to adopt EHR systems, health information exchanges do not have a record of success.14 In one survey, about half the states reported having trouble finding a way for it to be economically sustainable with the initial federal financing ending.15 Others have had trouble gaining widespread provider use. Health care industry leaders believe the state-based information exchanges have not worked and are looking to private organizations to step up, but concerns remain whether private efforts will achieve all public goals for information exchange.16
Interoperability and other issues with EHRs have led to frustration from patients and providers. Despite the desire to have convenient electronic access to personal health information, patients feel that state and federal privacy laws are not sufficient to properly protect their information from data breaches.17 Providers have also often found them to be time-consuming and frustrating.18 As a result, providers are still skeptical about how much these new tools can help improve patient care.19 Providers can also be afflicted with status quo bias, which is a preference for the current state of affairs and explains the strong tendency that they often have to remain with paper records or even an old EHR system when a newer one would be better.
Furthermore, the brain is built with sensitivity towards negative news, which is called negativity bias, providing another reason providers are quick to recall the negative aspects of EHRs. These negative experiences have slowed the full potential of EHRs, as physicians are frustrated with many issues and must wait for fixes to the issues they have encountered with EHRs.20
This failure to create effective, comprehensive EHRs has negative effects on patient care and on patients themselves. Studies show that lack of integration can lead to duplicative exams and procedures.21 In fact, one study estimates that at full adoption, ineffective EHRs could be responsible for 60,000 adverse events each year, mostly due to the inability of systems to communicate with each other.22 For example, according to a news report, a drug order “transmitted by an electronic app to a pharmacy using a different app” loses pertinent information in the process.23
On the positive side, integrated EHRs have been shown to deliver improved patient care and efficiencies: one study found that integrated EHRs could reduce the number of lab tests by approximately 6%.24 Moreover, EHRs were intended to facilitate the tracking of patients with chronic diseases and ensure those patients get the care they need to avoid expensive and repeated hospitalizations.25 The lack of integration between providers and hospitals frequently prevents that goal from being accomplished.26
Where are Innovations Happening?
Despite the many challenges, the basic task of exchanging health information has been succeeding in several places throughout the country. The California Integrated Data Exchange (Cal INDEX) is an independent, not-for-profit organization spawned by two leading health insurers in the state: Blue Shield of California and Anthem Blue Cross. While the two are competitors, they cooperated to provide startup funding for Cal INDEX because they can both benefit from improving care and lowering costs for their members by ensuring providers have access to patients’ complete health records.27 Cal INDEX is an example of a centralized health information exchange—it works by collecting information from any health plan, hospital, and doctor in California that wants to contribute and receive information.
All states have had health information exchange initiatives. The local examples memo describes the status of each one.
By using claims data from insurers, Cal INDEX can identify missing clinical information. For example, if a patient’s record shows a claim for a treatment of allergic reaction, then that information can be used to alert providers to identify missing information like the source of the allergy, which could be an antibiotic as in Tracie Storie’s situation, described above. Cal INDEX will be funded through subscription fees collected from groups sharing data.28 It will initially provide records for 9 million Californians, about one quarter of the state’s population.
Established in 2009, the Georgia Health Information Network is another network that connects regional health information exchanges as well as hospital systems, physician groups, and individual practitioners. It has more than 16 million patient records accessible to providers. It is an example of a decentralized model because it merely exchanges information between sources rather than stores the information in one place. It recently announced the first cross-state connection of two health information exchanges with the South Carolina Health Information Exchange. It will support residents of both states as they move between the states and large metro areas like Atlanta and Columbia.29
There have also been successful efforts in rural states. For example, the Arkansas State Health Alliance for Records Exchange (SHARE) is a state-wide health information exchange created and maintained by the Arkansas Office of Health Information Technology. All Arkansas hospitals and 60% of office-based physicians use EHRs, but those systems are not interoperable. Using secure connections, SHARE creates an index of patient records from multiple sources and uses the index to let providers see and receive information about each of their patients for the care they receive elsewhere.30 It accommodates providers who have not adopted EHRs through a virtual health record option that gives them access to their patients’ information stored electronically elsewhere. SHARE also provides direct secure messaging for participating providers with or without an EHR. SHARE includes nearly 900,000 unique patient records, 26 participating hospitals, and 244 participating practice sites covering 95 Arkansas cities.31 Several other states including Georgia, Indiana, and Nebraska have also recently started their own EHR pilot projects focused on giving patients access to a complete electronic health record.32
Since January 2013, patients within the Veterans Administration (VA) health care system can download their medical records and share them with their health care providers using “Blue Button.”33 A recent study has shown that VA patients have found the Blue Button helpful because they could better understand their health history by having their information in one place.34 The study also found that educational efforts are necessary to increase awareness of the benefits of using Blue Button.35
Dossia, a health information technology service, has similar ambitions for employees of private companies. Intel, Pitney Bowes, Walmart, and other Fortune 500 companies helped launch this service that combines a patient’s medical information from multiple sources into one account.36 Although employers provide Dossia as a benefit to employees, it keeps personal data independent from the employer; employees control who has access to their records. It also lets patients give doctors a complete medical history without forgetting or mixing up key details.
Complete records make it more efficient for companies like IBM to use EHRs to improve the quality of health care. Recently, IBM announced that it would use its supercomputer Watson and collaborate with Anthem to improve patient care. Watson will be used to aid physicians in identifying the optimal treatment options for patients.37 Watson accomplishes this by sifting through comprehensive patient records and medical research, analyzing this data, and “identifying key pieces of information across many different cases.”38 Another promising example of the use of complete records is Apple’s development of HealthKit, a partnership with Epic, a large EHR company, to sync provider health records with patient mobile applications.39 Patients will then easily be able to share their information with providers when necessary.
How Can We Bring Solutions to Scale?
Every Medicare and Medicaid beneficiary should have a complete electronic health record—provided through a health information exchange and financed by savings from eliminating wasteful care. Doing this would give every beneficiary a “personal health record,” which contains their insurance and clinical data as well as the opportunity to add their own data from health-related devices like Fitbits, mobile phones, and scales with Bluetooth capability.40
This could be done through either a centralized or decentralized model.
The centralized model is sometimes called a health record bank (HRB), which is “a private, independent organization that provides a secure electronic repository for storing and maintaining an individual’s lifetime health and medical records from multiple sources and assuring that the individual always has control over who can access their information.”41 Think of your checking account at a local bank: various entities can make deposits into your account once you give them permission—from your job depositing your paycheck to the federal government depositing your tax refund. And you can access your account anywhere—from online to at a nearby ATM—since the entire system is on a common platform and linked together. The estimated costs of geographically-based HRBs are only $8 per year per account, depending on the number of prescribers.42
Smart phones may provide the missing link for consumers to take charge of their health records. Imagine that your phone can let you avoid filling out your medical history every time you go to the doctor.43 Or it can help you keep up with taking your medications through text message reminders. Or let you keep your doctor informed on your daily exercise progress. Indeed, Apple’s Health Kit, which is part of every new iPhone, and similar apps in other smart phones, can do all that and more.44 The potential uses and benefits may well be enough to overcome consumers’ natural reluctance to help manage their own health information.
A decentralized health information exchange would also qualify for funding as long as it provided patients with a personal health record. Although such exchanges have not commonly developed that ability, it would be critical in helping insure the portability of a patient’s information as they move from between centralized and decentralized systems. For example, if a person moved from Georgia to California and had been enrolled in the George Health Insurance Exchange, that person would need to download his/her Georgia information and upload it into the centralized Cal INDEX in California.
A personal health record can be used to collect data to prevent congestive heart failure through wireless, remote monitoring devices for a patient’s weight and blood pressure. Such monitoring has proven successful in preventing costly hospital stays to treat heart disease—saving money and leading to happier, healthier patients.
Through both centralized and decentralized models, providers and plans could still retain (and use) the original records they generate, but the exchanges would assemble and maintain a complete and unaltered copy of the patient's medical records, including diagnoses, treatment history, test results, allergies, and prescriptions. They also provide patient “account holders” with standardized processes for granting third parties, such as providers or researchers, access to all or part of their records.
Privacy and security concerns over an EHR system could arise as a result of digitizing records. However, the patient control feature of the information exchanges works to alleviate some of these issues—privacy can be protected because any access to records held by the information exchange requires specific patient consent. And a centralized health record bank serves as the legal agent of the patient, responsible for gathering and guarding the patient's records. In contrast, the information generated for EHRs by providers legally belongs to the provider under copyright laws.
To achieve provider and health plan participation in data sharing, a decentralized model must work hard to gain the cooperation of a provider for exchanging information. For the health record bank approach, it can ensure participation by leveraging the Health Insurance Portability and Accountability Act (HIPAA) requirement that providers supply patients with copies of their records upon request.45 Although not well known, the HIPAA privacy rule stipulates that if records exist in electronic form, they must be delivered in electronic form. That requirement was reinforced in the American Recovery and Reinvestment Act (ARRA) of 2009 and is being promoted by the more recent Blue Button initiative that will allow VA and Medicare patients to retrieve their health records electronically.46 There is also a regulatory rule being formulated that would allow patients to request their laboratory results directly.47 Blue Button will be one way that providers can make “deposits” of a patient’s information into a health record bank.48 It will give patients a more complete health record as deposits of information are made from the various providers that a patient sees.
For people not in Medicare of Medicaid, the incentives for health plans to offer a personal health care record should be strong enough to create information exchanges without further public investment. But, if needed, Congress could guarantee all Americans access to a personal health record by including it as part of the essential benefits package.
Ultimately, the true measure of success of any system that provides a lifetime health record is how useful it is to patients and their providers. Congress should link public payments for lifetime records to simple tests of functionality and utility. For example, a fully functional system can display data from multiple sources in a graph that charts a patient’s progress over time.49
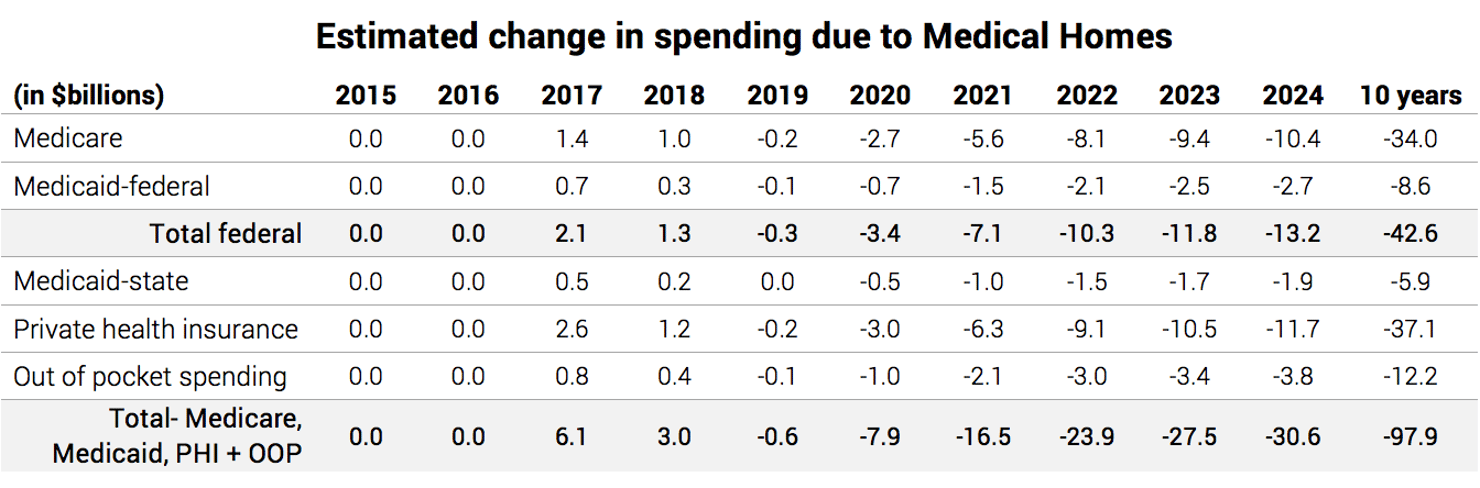
Potential Savings
Personal health records and their uses have been shown to produce substantial savings from a reduction in duplicative services and other cost savings like refilling prescriptions digitally. One study found major savings with reduction in laboratory tests, drug utilization, radiology exams, and reduction in length of hospital stays.50 Although this study predates the widespread use of electronic health records in hospitals and physician offices, the results remain relevant because they depend on sharing the information in EHRs among providers, which is not occurring despite the digitization of health care records. A summary of the potential savings is shown below.
Federal savings from this proposal total $41.7 billion over ten years. States will save slightly over $5 billion. And private health insurance and individuals will save another $50.9 billion over ten years.
Questions & Responses
What kinds of organizations can operate health information exchanges?
A decentralized exchange or a health record bank could be chartered by a variety of organizations that already have a connection with patients. Physician groups, employers, and health plans could provide access to an exchange or health record bank. But the exchange or bank itself would have to follow strict rules to keep it independent by giving patients control over who has access to their data, storing that information securely, and ensuring the information can be readily transferred to another health record bank at the patient’s request.
Isn’t it risky to let patients control what information their physician can see?
Patients already exert control over the information they give to doctors. For example, they may pay cash for a service to keep it out of the insurance system. Moreover, patients cannot control what doctors see in their own records about their patients. Today, doctors mostly operate in the dark about the care their patients receive elsewhere because health information is not integrated across care settings. This lack of sharing is the current state of affairs even though federal law allows providers to share data about patients without the patient’s permission for routine care and other purposes. Trusting patients with their own information has the potential to increase a their confidence in data sharing because they can control where it goes.
Isn’t having all of a patient’s records stored in one location a security risk?
Any computerized system has security risks. But computer experts have long recognized that it is easier to secure a single location of data than multiple sites of data that must constantly pair up those data to create a complete record.51 A health record bank or a decentralized exchange would be directly accountable to patients for the security of the data. If the bank or exchange fails to protect data even under strict regulations for security, then patients should be free to find another place to store their records.
Could a health record bank sell services to patients based on their data?
With a patient’s explicit permission, a health record bank or a decentralized exchange could offer their member a variety of services ranging from wellness programs and prevention reminders to recommendations for clinical research trials. One particularly valuable service would send an alert to a patient’s loved ones if he or she ever showed up at the emergency room unconscious.52 The revenue from such services would help offset the costs of collecting and organizing medical records from health care providers.
What about the Massachusetts eHealth Collaborative? Didn’t it fail to produce savings?
Yes, the Massachusetts eHealth Collaborative was a high profile pilot program to digitize and link together the medical records of hospitals and physicians in three communities in Massachusetts.53 Although it produced some savings in outpatient health costs, overall inpatient costs did not fall as expected.54 But this collaborative was not built on a complete record for every patient. Instead, it only transmitted information between EHRs. No one had the responsibility to assemble a complete record for each patient. It is likely the savings would have been significant if all the EHR systems had access to a complete record for each patient.55


