Report Published March 27, 2024 · 9 minute read
Same Service, Same Price: Tackling Hospitals’ Add-On Facility Fees
Darbin Wofford

Takeaways
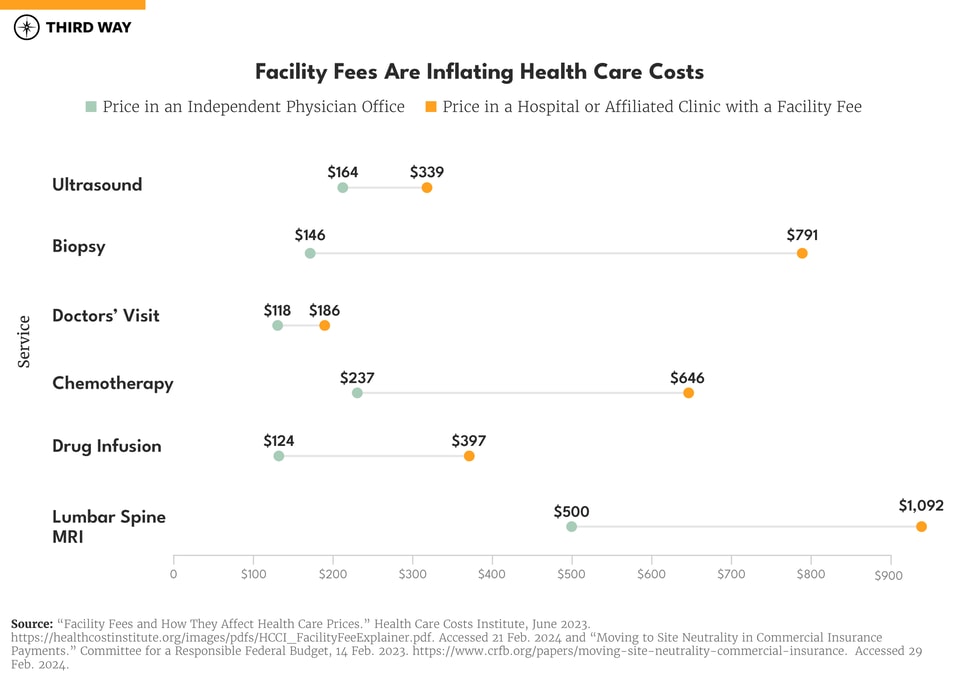
Patients are paying double for ultrasounds performed in hospitals. Some cancer patients are paying triple for chemotherapy infusions. The reason? Hospitals often add a “facility fee”—an extra charge just for walking in their doors.
Patients should pay the same price for the same service, and that starts by significantly limiting facility fees for private health coverage. Congress can do that through three steps, resulting in taxpayer savings of almost $300 billion over a decade.
Here's how:
- Ban hospitals from billing facility fees from their off-site clinics.
- Prevent facility fees for straightforward care within the hospital.
- Limit the size of remaining facility fees.
Imagine shopping at a supermarket and getting charged one bill for groceries and another just for entering the store. That would never fly, and no one would go there. Unfortunately, that’s exactly what hospitals are getting away with. Hospitals add a “facility fee” for the same services that an independent doctor’s office does for less. Because of that, the price patients pay for health care can depend more on where patients receive their care more than the quality of care it provides for a patient’s health.
For example, an ultrasound done in a doctor’s office costs $164 on average compared to $339 when provided in a hospital.1 Just seeing a doctor costs $118 in an independent physician’s office compared to $186 in the hospital. Despite some services being low-cost, such as routine labs and injectable drugs, hospitals can charge more by adding on facility fees for the same service. The ability to charge facility fees also incentivizes hospitals to take over physician practices, integrate them into their system, and dominate the health care market.
The solution: limit the use of facility fees in order to align the cost of standard care between hospitals and physician practice, where patients pay the same price for the same service. In this report, we examine the issues surrounding facility fees and three key steps to end the practice for good.
This report is part of a series called Fixing America’s Broken Hospitals, which seeks to explore and modernize a foundation of our health care system. A raft of structural issues, including lack of competition, misaligned incentives, and outdated safety net policies, have led to unsustainable practices. The result is too many instances of hospitals charging unchecked prices, using questionable billing and aggressive debt collection practices, abusing public programs, and failing to identify and serve community needs. Our work will shed light on issues facing hospitals and advance proposals so they can have a financially and socially sustainable future.
The Problem: Facility fees are jacking up medical bills.
Hospitals are mostly known for providing inpatient care, meaning overnight stays, complex surgeries, and treatment for severe illnesses and injuries. However, hospitals also provide outpatient care, such as evaluations and treatment for symptoms and tests that do not require an overnight stay. In fact, health care has been trending away from inpatient hospital stays and towards outpatient care over time.2 Patients typically receive outpatient care from a doctor’s office but may also go to a hospital or hospital-owned clinic.
Enter facility fees.
As patients enter a doctor’s office for a checkup or treatment, it is unlikely they will know whether that office is independently owned or part of a larger hospital system. To date, over half of the country’s doctors are hospital employees, a percentage that grows every year.3 After receiving medical care, patients receive a bill from the provider. However, if a patient visited a hospital or affiliated clinic, they may see a separate bill or charge for a “facility fee.” This fee is an extra charge tacked on by the hospital just for walking through their doors.
Hospitals have been billing facility fees since at least 2000.4 They claim their purpose is to cover “direct and indirect costs that allow a hospital to continue to provide services to patients.”5 While this could be true for more complex outpatient procedures occurring within the hospital, this argument doesn’t work in cases of labs, tests, telehealth, and consultations. Doctor’s offices owned by hospitals provide the same services as independent physician practices, but at a much higher price.
Facility fees are not always billed as a separate item, making things even more confusing. In negotiations between hospitals and health plans, facility fees can be part of the overall reimbursement price. However, regardless of whether facility fees are a separate line item or part of the price, hospitals charge an outsized amount compared to a physician office. For example, cancer patients pay nearly three times more for chemotherapy in a hospital, $646 for a one-hour chemotherapy infusion versus $237 in a physician’s office.6
The presence of facility fees leads to higher costs for patients—projected at $70 billion over the decade.7 Patients with private coverage are normally responsible for some levels of cost-sharing, and facility fees inflate their out-of-pocket costs. And, if a patient’s deductible is not yet met, they could be responsible for the entire facility fee.
Facility fees also cause higher premiums. Costlier charges billed to patients’ insurance put upward pressure on premiums. For employers, higher premiums mean more in health care expenses, leaving less room for wage growth and investments for growth.8
For the 25 million people lacking health insurance, facility fees can be especially devastating. If an uninsured patient goes to a hospital or one of their clinics, they will be responsible for the entire facility fee.
Beyond increasing prices for patients, facility fees are indicative of a broader, system-wide issue that exists throughout the health care ecosystem—incentives are often completely misaligned. The ability to charge facility fees, for example, incentivizes hospitals to take over physician offices to enlarge their dominance in the health care market. As more physician practices fall to big hospital chains, patients fall victim to more facility fees that fuel hospitals’ bottom lines.
Also, it should be noted that billing extra for straightforward care is not limited to patients with private insurance. In Medicare, the government pays hospital-owned clinics more than physician practices for the same services. For example, Medicare reimburses hospital-owned clinics $91 for a chest x-ray compared to $26 in a physician’s office.9
The Solution: Take an axe to hospitals’ facility fees.
Patients should pay the same price for the same service, and that starts by significantly limiting facility fees for private health coverage. Several states have led the way by either banning facility fees directly or placing limits and transparency requirements on the practice.10 Congress is also considering steps to limit facility fees. The Senate Health Committee passed the Bipartisan Primary Care and Health Workforce Act, introduced by Chairman Bernie Sanders (I-VT) and Senator Roger Marshall (R-KS), which would require transparent billing by hospital-owned clinics and banning facility fees for telehealth and evaluation/management services.11
Congress should go even further and protect patients with private insurance from burdensome facility fees. That would require three steps:
First, ban facility fees from off-site hospital clinics. These clinics include any hospital outpatient department located separate from the hospital’s primary location. The package passed by the Senate Health Committee includes a ban on facility fees for telehealth and evaluation/management services, but an earlier iteration of the bill would have banned facility fees for all off-site clinics. In his most recent budget request, President Biden proposed to ban facility fees for telehealth and other outpatient services.12
In his most recent budget request, President Biden proposed to ban facility fees for telehealth and other outpatient services.
Second, prevent facility fees for straightforward care within the hospital. While some complex care may warrant an additional charge if done at a hospital, most outpatient care should cost the same whether it’s being done at a hospital or physician office. That is why Congress should ban facility fees for services where there is no cost difference to the provider. This includes primary care, telehealth (where the doctor works within the hospital), and low-complexity services.
Third, limit the size of remaining facility fees. Facility fees are not always separate bills; sometimes they are hiding in prices negotiated between hospitals and insurers. Congress should cap the amount charged by hospitals for outpatient care to the amount charged for the same service in nearby physician offices. Hospitals should also be prohibited from billing facility fees separately from services.
In addition to tackling facility fees, Congress must also remove the incentives in Medicare that encourage hospitals to take over physician practices. Aligning payments in Medicare to reimburse hospitals and physicians the same levels for outpatient care would lower costs for seniors and strengthen insurers’ ability to negotiate down facility fees.
The Savings
Limits on facility fees, in addition to aligning payments in Medicare, would result in significant savings for patients, employers, and taxpayers.
According to a Committee for a Responsible Federal Budget study, limits on facility fees for those with private coverage would save patients $73 billion in cost-sharing over a decade. Premiums would decline by $386 billion, applying to both workers and their employers, which would increase wage growth and investment. Overall, taxpayers would save $117 billion.13
Aligning payments in Medicare would also produce significant savings, with seniors and those with disabilities saving $137 billion over the decade. Taxpayers would save of $175 billion, and the private market would save somewhere between $140-$466 billion due to more negotiating power for patients’ health plans with hospitals.14
Together, taxpayer savings from Medicare reforms and limits to facility fees amount to nearly $300 billion over a decade. Because there are many needs through the health care system, Congress should use these savings to strengthen patient access and affordability and invest more funding towards safety net hospitals, specifically those serving high levels of uninsured patients and those enrolled in Medicaid and the Children’s Health Insurance Program.15
Conclusion
Through charging facility fees for straightforward care, hospitals are increasing patients’ costs while driving up premiums for individuals and employers. Hospital acquisitions of physician offices are suppressing competition, increasing prices even further. Congress should act now to limit facility fees and address incentives for consolidation in health care.
To learn more about lowering hospital costs in Medicare, click here.

