Explainer: The Cassidy-Hassan Hospital Reform Bill

Toward the end of 2024, Senators Bill Cassidy (R-LA) and Maggie Hassan (D-NH) released a legislative framework to reduce the cost of hospital care and bridge the gap between have- and have-not hospitals. They noted that “While many factors drive health spending, rising health care costs have in part resulted from an increase in consolidation among hospitals and outpatient care settings.”1
Their approach has two main strategies: reforms ensuring patients pay the same price for the same service, and a reinvestment of savings into rural and high-need hospitals. Below, we explore the Cassidy-Hassan proposal and the issues they seek to address:
Same Service, Same Price Payment Reform
The Problem: Right now, hospitals get paid more for routine care than independent physicians—even for the exact same service. Due to this dynamic, hospital systems are acquiring physician practices, resulting in less competition and higher patient costs. As a result, seniors are paying higher prices for the same services, such as doctors’ visits, telehealth services, physician-administered drugs, and other common services. In addition to higher payments from Medicare, hospital-owned practices will often bill patients “facility fees” that inflate costs for patients with private insurance. A study conducted by the Actuarial Research Corporation found that site neutral payment reform would save Medicare $138 billion over the next 10 years and lower out-of-pocket costs for Medicare beneficiaries by $21 billion over the same period.
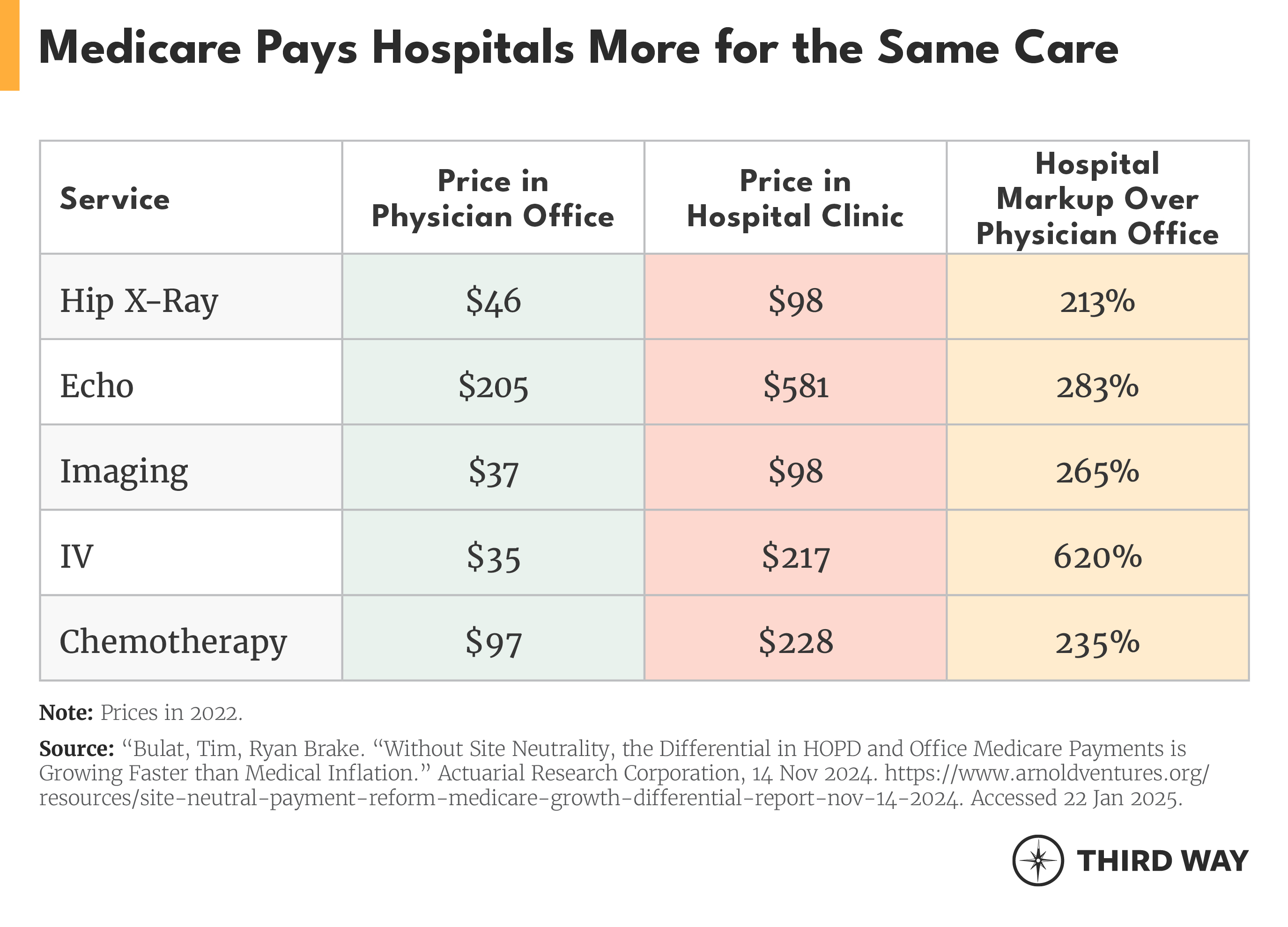
The Cassidy-Hassan Approach: The Cassidy-Hassan proposal embraces what’s called site-neutral payment reform, where Medicare sets payments at the same price for the same service—whether it was provided in a hospital-owned clinic or independent physician practice. Congress pursued this policy in the Bipartisan Budget Act of 2015, but it just applied to 1% of services because it only covered new clinics. It exempted existing clinics and physician practices that are acquired by hospitals and incorporated into the hospital system.
Sens. Cassidy and Hassan would extend site-neutral policies to all hospital-owned clinics not located on hospital campuses. The hospitals that would see the largest reductions in payments due to this policy are those that are the most consolidated, meaning large systems as opposed to smaller hospitals with limited market power.
The framework would also extend site-neutral payments to services provided on a hospital campus for services that are safely and commonly performed in hospital outpatient departments, ambulatory surgical centers, and physician offices. This proposal would require the Secretary of Health and Human Services to identify these procedures using four years of data, identify the site of care where each procedure was most frequently performed, and set their payment rates to the site of care with the highest volume.
These reforms would produce significant savings for patients. Expanding site-neutral payments would save up to $94 billion for seniors through lower cost-sharing and premiums. Patients with private insurance would see savings too. Because prices paid by commercial payers are largely based on Medicare, site-neutral payments would give payers justification to negotiate lower prices for outpatient care, resulting in lower premiums and out-of-pocket costs. Hospitals would also be less incentivized to consolidate if care is provided in the lowest-cost setting, allowing payers to negotiate lower prices.
Supporting Rural and High-Need Hospitals
The Problem: Hospitals serving rural and low-income communities are struggling with inequities increasing between have and have-not hospitals. More than 700 hospitals are at risk of closing, and, in the past decade, more than 100 rural hospitals have closed. Rural hospitals especially struggle due to low patient volume, high labor costs, and a higher Medicare and Medicaid payer mix. And if a rural hospital closes, patients could be hours away from the next nearest hospital and emergency room. Along with risk of closure, these hospitals are vulnerable to takeovers by big systems. In some cases, hospital chains will acquire a struggling rural hospital and scale down services.
So-called “safety-net hospitals” that serve low-income populations face their own unique challenges. Low-income communities have the largest number of patients enrolled in Medicaid, which mostly pays less than Medicare and private insurance. Currently, just 7% of hospitals serve one-third or more patients with Medicaid coverage. Current payment structures in Medicare and Medicaid fail to lift up the hospitals that need it most.
While rural hospitals often face declining revenue, site-neutral payment reforms would not substantially affect their levels of reimbursement. For example, a recent study by Avalere indicated that 2.3% of hospital outpatient Medicare revenues are subject to the site-neutral provisions of current site-neutral payment policies (i.e., the Balanced Budget Act of 2015). The study also noted that rural hospitals account for a much smaller share of Part B spending compared to urban hospitals (10.8%) and that rural hospitals use off-campus clinics less than urban hospitals. Importantly, site-neutral payments would not impact rural hospital reimbursement directly, only the Medicare Part B revenue generated from off-campus clinics. Facilities that do not meet the definition of off-campus outpatient departments (e.g., dedicated emergency departments, on-campus outpatient departments, remote hospital locations, Critical Access Hospitals, Rural Emergency Hospitals, and Rural Health Clinics) will continue to be exempt from site-neutral payment requirements.
The Cassidy-Hassan Approach: The Cassidy-Hassan framework would reinvest the federal savings from site-neutral payment reform in order to close the gap between have- and have-not hospitals. First, it would increase funding for different types of rural hospitals.2 It would also define other “high needs” hospitals not located in rural areas. These hospitals would be in urban or suburban areas, have dedicated emergency rooms, and could be eligible for reinvestment of site-neutral savings. But they must have high percentages of Medicare and Medicaid patients and provide high levels of uncompensated care. The framework does not yet specify what those levels are.
The framework also would invest in specific medical services, encouraging hospitals to offer these services through bonuses. These services include trauma centers, emergency psychiatric services, and burn units.
Lastly, the framework would incentivize hospitals to participate in value-based care arrangements. These payment models encourage hospitals to put quality over quantity by rewarding them for meeting quality benchmarks and increasing efficiency. The Cassidy-Hassan framework includes two separate alternative payment (APM) arrangements.
Under the first APM option, hospitals currently in two-sided risk advanced alternative payment models (AAPM) (or hospitals that choose to enter an AAPM) would receive higher payments per member per month. The framework also includes an option where hospitals could receive payment adjustments for inpatient days attributable to any APM.
Under the second APM option, rural and safety net hospitals could enter Accountable Care Organizations that set the Medicare spending benchmark based on the time period before site-neutral payments are implemented. Under this option, the model would begin as a one-sided risk model for two years and transition to a two-sided risk model beginning in the third year and the pre-site-neutral benchmark would phase out over time.
Call for Action
In this new Congress, the Senate Finance Committee should act to take up this legislation. It’s been endorsed by a variety of organizations, including think tanks on the left and right, consumer advocates, provider groups, and employers.
Endnotes
https://www.cassidy.senate.gov/wp-content/uploads/2024/10/Site-Neutral-Policy-Framework-Final.pdf
These hospitals include Sole Community Hospitals (i.e., hospitals that are located more than 35 miles from other hospitals, or are located in rural regions and meet other conditions certain conditions related to market share and distance), Low-Volume Hospitals (i.e., hospitals that are more than 25 road miles from another hospital and have fewer than 200 total discharges.), and Medicare Dependent Hospitals (i.e., hospitals that are located in rural regions, have 100 or fewer beds, are not Sole Community Hospitals, and at least 60% of inpatient days or discharges are from patients entitled to Medicare Part A benefits).
Subscribe
Get updates whenever new content is added. We'll never share your email with anyone.
