How Hospitals are Raising Drug Prices

Takeaways
Patients are paying more to hospitals for physician-administered drugs like chemotherapy and other cancer treatments. Hospital systems’ growth in market power is leading to larger markups for outpatient drugs, where patients pay three to seven times more than in other settings of care. Meanwhile, nearly half of hospitals that qualify for substantial discounts through the 340B Drug Pricing Program are using discounts to further consolidate their market power, rather than making these drugs more affordable for low-income patients.
Congress should take action to alleviate the burden of high drug costs on hospital patients by:
- Limiting hospital mark-ups for outpatient drugs.
- Reforming the 340B Program to improve access for patients.
- Reducing 340B’s incentives for hospitals to consolidate.
There is a missing piece to the front-page debate over prescription drug prices. While patients regularly pick up prescriptions at the pharmacy, many drugs are administered by physicians in a hospital or doctor’s office. Depending on where these drugs are administered, patients could be left paying a lot more than they should.
For example, a single round of chemotherapy costs patients over $600 in a hospital or hospital clinic, on average. But it costs three times less in an independent physician’s office.1 This disparity is due to consolidation in the hospital industry, where hospital systems buy up other hospitals and physician practices to gain market power and charge higher prices. And contributing to that consolidation is the 340B Drug Pricing Program, which requires prescription drug manufacturers to give hospitals discounts on drug purchases.
To reduce the cost that patients pay for drugs, Congress must take action. In this report, we lay out how hospital drug mark-ups are hurting patients and offer a variety of policy solutions.
This report is part of a series called Fixing America’s Broken Hospitals, which seeks to explore and modernize a foundation of our health care system. A raft of structural issues, including lack of competition, misaligned incentives, and outdated safety net policies, have led to unsustainable practices. The result is too many instances of hospitals charging unchecked prices, using questionable billing and aggressive debt collection practices, abusing public programs, and failing to identify and serve community needs. Our work sheds light on issues facing hospitals and advances proposals so hospitals can have a financially and socially sustainable future.
The Problem: Hospitals are raising drug prices.
Most medications are self-administered by an individual patient—think over-the-counter pills or something you pick up from a pharmacist. Injectable medicines are often different, though. Some, like insulin, can be administered by a patient, but most injectables and infused drugs are administered by health care professionals in doctors’ offices or hospitals.
Here’s how that works: most hospitals purchase drugs and then charge patients and their insurance. This is known as “buy and bill” reimbursement. For patients covered under Medicare, the price is fixed, based on Medicare’s fee schedule. However, for private insurers and employer plans, prices vary considerably. Each plan negotiates individually with hospitals, and hospitals’ market power can greatly affect the cost of these drugs.
The problem is that, under our current system, prices for hospital-administered drugs are increasing, resulting in higher costs for patients. Hospitals are marking up prices for physician-administered medicines by 300-700%.2 For example, New York-Presbyterian Hospital in New York City has pushed mark-ups to the extreme with a $55,000 price for the cancer drug Neulasta for commercially insured patients. That is 12.5 times the average price in Medicare. From 2008 to 2021, Medicare patients saw their prices for hospital-administered drugs increase by 14% a year, on average. Meanwhile, the same drug prices in physician offices grew by 7%.3
Hospitals are marking up prices for physician-administered medicines by 300-700%.
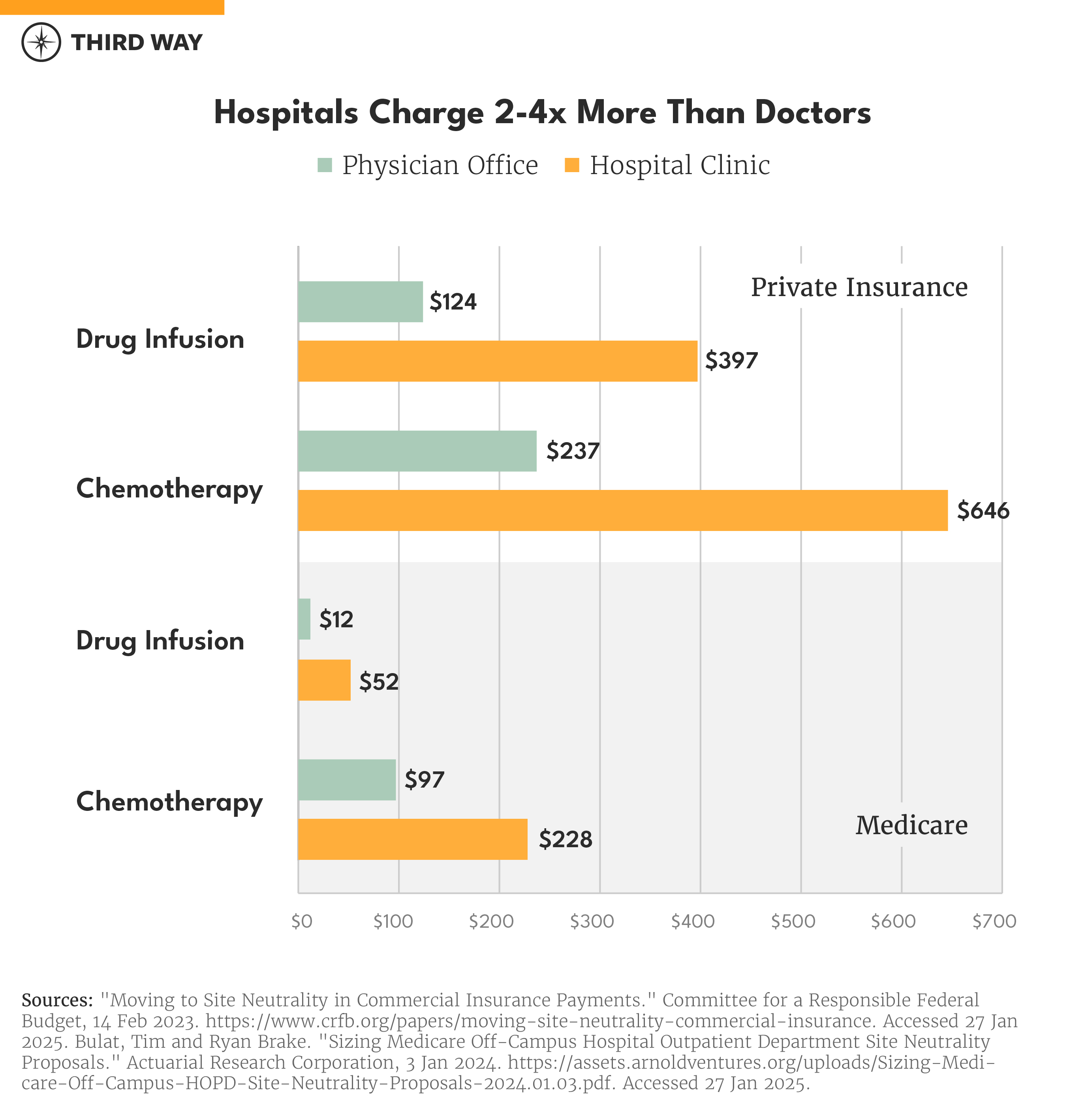
Another factor making the problem worse is the rising trend of hospitals acquiring physician practices. The majority of physician-administered drugs are provided in hospitals and their affiliated clinics—as opposed to independent doctor offices.4 That’s an issue because Medicare pays hospital-owned clinics between two to three times more for drug administration services compared to independently-owned physician offices.5 This means seniors with cancer are paying hundreds of dollars more for their chemotherapy if their doctor happens to be employed by a hospital instead of practicing independently. There is also a significant price difference for patients with private insurance, for whom a drug infusion costs 3.2 times more and chemotherapy costs 2.7 times more in a hospital setting.6
Because health plans and the patients they cover are responsible for paying most of those drug costs, some have implemented strategies to reduce those prices. For example:
- Some health plans require patients to purchase a drug from a specialty pharmacy and bring it directly to the hospital for administration. This process is known as “brown bagging.” It takes hospitals out of the equation for purchasing drugs to prevent high mark-ups but requires patients to transport drugs to physician offices. It does, however, lower patient cost-sharing.
- Another strategy for health plans is to contract with a specialty pharmacy to ship the medication to the hospital. This is known as “white bagging.”7 This process is less of a burden for patients compared to brown bagging, but, unfortunately, several states have enacted laws to limit white bagging and preserve hospitals’ power to inflate drug prices.
Hospital prices increase due to consolidation.
Consolidation plays a primary role in driving prices up for health care. When hospitals gain more market power, they can charge health plans high prices due to the lack of competition. Since two-thirds of hospitals are now part of a consolidated health system and 60% of physicians are employed by hospitals, it’s no wonder prescription drug prices have risen along with hospital mergers and acquisitions.8
High prices due to consolidation are not limited to hospital-administered drugs. Other services such as routine doctor visits, labs and tests, and minor procedures are significantly more expensive in hospital systems than independent offices.9 As prices rise for drug administration and other hospital services, patients are left behind with higher costs. Employers providing health insurance benefits to over half of Americans must raise premiums to pay these higher prices, and patients’ out-of-pocket costs increase.
As prices rise for drug administration and other hospital services, patients are left behind with higher costs.
One major driver for consolidation is the 340B Drug Pricing Program. The program, created in 1992, requires prescription drug manufacturers to give eligible health care providers discounts on medications, where hospitals keep the difference between the discounted price and what they charge health plans.10 It is an essential program that gives financial hospitals and other health care providers operating in low-income communities. However, 340B is failing to extend drug affordability to patients in hospitals enrolled in the program. Due to massive growth in the last decade, 340B is the second largest federal drug program behind Medicare Part D, and greater than Medicare Part B and Medicaid.11
For an overview of the 340B Drug Pricing Program, click here.
The 340B Program has proven to be very lucrative for hospitals, providing $60 billion in discounted sales annually. Because of that, hospitals increasingly look to maximize these discounts through mergers and acquisitions. When a 340B hospital acquires a clinic or physician office, they may convert them into a 340B “child site.” These sites become eligible to receive 340B discounts from drugs prescribed to their patients. However, the bulk of child sites are located in wealthier, and less diverse communities with a higher number of commercially-insured patients.12 Because their insurance pays more for drugs than Medicare and Medicaid, they are more lucrative to hospitals—the more expensive the drug, the larger discount they get to keep. In their policy approaches to reduce the cost of care, the Congressional Budget Office highlighted 340B’s role in driving consolidation.13
Unlike other health care providers in 340B, like community health centers and Ryan-White clinics, hospitals have no requirement to share discounts with patients. Instead, they’re inflating prices for those low-income patients. A recent study from the UC Berkley School of Public Health found that hospitals in the 340B program are charging 300% of the cost of what they paid for infusion drugs.14 According to a report from the North Carolina State Treasurer last May, hospitals are charging patients 3.5 times the acquisition cost of cancer drugs. For 340B hospitals in North Carolina, though, the mark-up is 5.4 times the hospitals’ cost.15 Another study found that 340B hospitals are marking up cancer drugs up to 11 times.16
Unlike other health care providers, like community health centers and Ryan-White clinics, hospitals have no requirement to share discounts with patients.
The Solution: Lower drug prices through hospital payment reforms.
Congress needs to reform the system that incentivizes hospitals to inflate the cost of drugs. Whether a drug is picked up at a pharmacy counter or administered by a doctor, patients need relief. Below, we outline three areas where Congress can protect patients from paying too much for drugs administered in hospitals:
First, limit hospital high prices for outpatient drugs. In hospitals and their affiliated clinics, physician-administered drugs should cost patients the same amount as an independent physician’s office. The Lower Costs, More Transparency Act would make that the case for patients visiting hospital outpatient departments located separate from the main hospital campus. That bill passed the House last Congress and would have saved Medicare $3.7 billion over a decade if enacted into law. Congress should also go further and apply this policy to outpatient departments located on a hospital’s campus. This expanded approach is part of a proposal from Senator Bill Cassidy (R-LA) and Maggie Hassan (D-NH).17 Beyond Medicare, patients with private insurance should also be protected from paying inflated prices by limiting the use of hospital facility fees for outpatient care.18 These policies would reduce, in part, hospitals’ incentives to buy up physician practices.
Second, reform the 340B Drug Pricing Program to improve access for patients. Hospitals who are part of 340B should have the same requirements as other providers, like community health centers, to ensure patients are benefiting from the program. The 340B Affording Care for Communities & Ensuring a Strong Safety-Net (ACCESS) Act, introduced last year by Representatives Larry Bucshon (R-IN), Buddy Carter (R-GA), and Diana Harshbarger (R-TN), would require 340B hospitals to provide minimum levels of charity care to low-income patients and ban the use of aggressive medical debt collection practices.19 Under this legislation, patients up to 200% of the federal poverty level would qualify for charity care based on a sliding scale. The bill’s provisions would apply to prescriptions made by 340B hospitals and were picked up by the patient at the pharmacy counter. Patients would also be protected from hospitals’ use of aggressive medical debt collection practices, such as suing patients and garnishing their wages, under the 340B ACCESS Act.
Third, reduce 340B’s incentives for consolidation. If a hospital-owned clinic is going to be eligible as a 340B child site, it should have stronger standards for participation. The 340B ACCESS Act would create standards to serve low-income communities to ensure clinics in wealthier and less diverse areas do not qualify for the program. Child sites under 340B would also need to meet the same charity care requirements as their parent hospital under this legislation and provide medical services beyond dispensing drugs.
What about rural hospitals?
When evaluating policies to reduce the cost of hospital care, policymakers need to ensure that access in rural communities does not suffer. As we’ve previously written, the Lower Costs, More Transparency Act’s provisions for reducing hospital payments for drug administration services would only affect 0.1% of rural outpatient spending.20 The legislation only applies to hospital-owned clinics separate from the hospital campus, which are less common in rural areas. Further, it would not take effect for rural hospitals for five years after the bill’s enactment. While the Cassidy-Hassan proposal applies to on-campus, outpatient locations, the framework includes significant investments in rural and other high-needs hospitals that would not only offset the minor reductions in payments but would leave them with more funding in total.
Under the 340B reform proposals discussed in this report, rural hospitals would abide by the same requirements as other 340B hospitals. As a result, patients living in rural areas would see lower costs. Meanwhile, the 340B ACCESS Act would expand the number of rural hospitals eligible for the program. Rural Emergency Hospitals, with the designation created in 2021 to prevent rural hospital closures, are not part of 340B. While hospitals are still obtaining this designation, more than 1,500 hospitals qualify, including Critical Access Hospitals, but the lack of 340B qualification might be a disincentive.21 This bill corrects that by including these hospitals in the program.
Conclusion
As health care costs continue to rise and become more burdensome for patients and American families, Congress should work to enact policies to make health care more affordable. Addressing high drug prices in hospitals should be a bipartisan effort.
With consolidation being a primary driver in rising health care costs, bolstering competition through the proposed reforms would lower out-of-pocket costs for patients, reduce the cost-burden for providing coverage for employers, and achieve significant savings to taxpayers.
Endnotes
Wofford, Darbin. "Same Service, Same Price: Tackling Hospitals’ Add-On Facility Fees." Third Way, 27 Mar 2024. https://www.thirdway.org/report/same-service-same-price-tackling-hospitals-add-on-facility-fees. Accessed 3 Feb 2025.
Herman, Bob. "Hospitals are making a lot of money on outpatient drugs." Axios, 15 Feb 2019. https://www.axios.com/2019/02/15/hospital-charges-outpatient-drug-prices-markups. Accessed 3 Feb 2025.
Nguyen, Nguyen X., et al. "Medicare Part B Drugs: Trends in Spending and Utilization, 2008-2021." Department of Health and Human Services, 9 June 2023. https://aspe.hhs.gov/sites/default/files/documents/fb7f647e32d57ce4672320b61a0a1443/aspe-medicare-part-b-drug-pricing.pdf. Accessed 3 Feb 2025.
Fronstin, Paul and M. Christopher Roebuck. "Location, Location, Location: Spending Differences for Physician-Administered Outpatient Medications by Site of Treatment." EBRI, 19 Aug 2021. https://www.ebri.org/docs/default-source/pbriefs/ebri_ib_536_locationx3-19aug21.pdf?sfvrsn=cf6c3b2f_4. Accessed 3 Feb 2025.
"Bulat, Tim and Ryan Brake. "Potential Impacts of Medicare Site Neutrality on Off-Campus Drug Administration Costs." Actuarial Research Corporation, 18 Oct 2023.
https://craftmediabucket.s3.amazonaws.com/uploads/Drug-Admin-Off-Campus-Site-Neutrality-2023.10.18.pdf. Accessed 3 Feb 2025.
"Same Service, Same Price: Tackling Hospitals’ Add-On Facility Fees."
"What is White Bagging?" MMIT. https://www.mmitnetwork.com/what-is-white-bagging/. Accessed 3 Feb 2025.
Kendall, David and Darbin Wofford. "Lowering Prices and Six Other Big Challenges for US Hospitals. Third Way, 30 Oct 2024. https://www.thirdway.org/report/lowering-prices-and-six-other-big-challenges-for-us-hospitals. Accessed 3 Feb 2025.
"Same Service, Same Price: Tackling Hospitals’ Add-On Facility Fees."
Wofford, Darbin and David Kendall. “Fixing a Critical Safety Net Program: 340B.” Third Way, 14 Nov 2023. https://www.thirdway.org/report/fixing-a-critical-safety-net-program-340b. Accessed 3 Feb 2025.
"340B Purchase Data Highlights Continued Program Growth." Avalere, 24 Oct 2024. https://avalere.com/insights/340b-purchase-data-highlights-continued-program-growth#:~:text=Among%20government%20sponsored%20and%20funded,prescription%20drugs%20in%20FY%202023. Accessed 3 Feb 2025.
Conti, Rena M. and Bach, Peter B. "The 340B Drug Discount Program: Hospitals Generate Profits By Expanding To Reach More Affluent Communities." Health Affairs, Oct. 2014. https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2014.0540?journalCode=hlthaff. Accessed 3 Feb 2025.
“Policy Approaches to Reduce What Commercial Insurers Pay for Hospitals’ and Physicians’ Services.” Congressional Budget Office, Sep 2022. https://www.cbo.gov/system/files/2022-09/58222-medical-prices.pdf. Accessed 3 Feb 2025.
"Study shows that hospitals impose major price markups on cancer and other specialty drugs." Berkeley Public Health, 14 Jan 2024. https://publichealth.berkeley.edu/news-media/research-highlights/study-shows-that-hospitals-impose-major-price-markups. Accessed 3 Feb 2025.
"State Treasurer Folwell Releases Report Finding North Carolina 340B Hospitals Overcharged State Employees for Cancer Drugs, Reaped Thousands of Dollars in Profits Per Claim." State Treasurer of North Carolina, 8 May 2024. https://www.nctreasurer.com/news/press-releases/2024/05/08/state-treasurer-folwell-releases-report-finding-north-carolina-340b-hospitals-overcharged-state. Accessed 3 Feb 2025.
Reed, Tina. "Hospitals mark up discounted cancer drugs at much as 11 times, report says." Axios, 13 Sep 2022. https://www.axios.com/2022/09/13/hospitals-cancer-drugs-mark-up-report. Accessed 3 Feb 2025.
"Cassidy, Hassan Release Policy Framework on Medicare Site-Neutral Reform to Lower Health Care Costs." Office of United States Senator Bill Cassidy, M.D., 1 Nov 2024. https://www.cassidy.senate.gov/newsroom/press-releases/cassidy-hassan-release-policy-framework-on-medicare-site-neutral-reform-to-lower-health-care-costs/. Accessed 3 Feb 2025.
"Same Service, Same Price: Tackling Hospitals’ Add-On Facility Fees."
"Carter, Buschon, and Harshbarger Introduce Legislation to Ensure Access and Transparency in 340B Drug Pricing Program." Office of United States Representative Buddy Carter, 28 May 2024. https://buddycarter.house.gov/news/documentsingle.aspx?DocumentID=11883. Accessed 3 Feb 2025.
Wofford, Darbin. " Lowering Hospital Prices while Protecting Rural Patients." Third Way, 12 Mar 2024. https://www.thirdway.org/memo/lowering-hospital-prices-while-protecting-rural-patients. Accessed 3 Feb 2025.
Schaefer, Sara L., et al. "The Emergence of Rural Emergency Hospitals." National Library of Medicine, 6 May 2023. https://pmc.ncbi.nlm.nih.gov/articles/PMC10163821/. Accessed 3 Feb 2025.
Subscribe
Get updates whenever new content is added. We'll never share your email with anyone.
