Report Published December 14, 2015 · Updated December 14, 2015 · 17 minute read
Local Examples: Innovations in Bundled Payments
Jacqueline Garry Lampert

More than half of physician revenue is based on fee for service payments, which incentivize physicians to perform more tasks rather than overseeing a patient’s overall care from beginning to end. These à la carte payments have led to substantial, and troubling, variation in price and quality for the treatment of similar conditions. This unstable, fee-for-service foundation for health care payment is set to remain in place for the foreseeable future, as even alternative payment models are built on this base.
The innovative concept of “bundled payments” attempts to reward value over volume by offering providers a fee for an episode of care. Often this set fee is a single payment to one provider or organization that is then responsible for compensating the other clinicians who have agreed to work together, rather than payers reimbursing unlimited claims for each of them. Bundled payments can save money over the fee-for-service system because the single payment encourages providers to think beyond their own role to the broader quality, value, and coordination of care a patient receives.
For example:
Nationwide
The Medicare Acute Care Episode (ACE) demonstration, a 3-year project which began in 2009 at five sites, provided hospitals with a single payment for both Part A services (hospital costs) and Part B services (physician costs) delivered during an inpatient stay. In addition to providing Medicare a discount below expected costs, this model also included provider and patient incentives and quality reporting requirements. The demo included only orthopedic and cardiovascular procedures. With Medicare silos broken down and Part A and Part B incentives aligned, costs at the ACE demonstration sites dropped mostly due to better contracting for devices and supplies. Costs were also lower because physicians followed stricter evidence-based protocols that prevented mistakes, eliminated duplication, and allowed physicians to share a portion of the savings they created. Overall, the ACE demonstration resulted in net savings to Medicare of $319 per episode, for a total savings of nearly $4 million.
Medicare’s Bundled Payment for Care Improvement (BPCI) Initiative, rolled out in August 2011, offers providers a choice of four bundled payment models that expand on the ACE experience. Among the models are one that focuses on care only within a hospital, two models that include inpatient care and care following discharge for a specific time period, and one that focuses directly on care after a hospitalization at nursing homes, community settings, or in the hospital if a patient is readmitted. For the last three models, Medicare has identified 48 episodes of care, which include 180 Medicare Severity Diagnosis Related Groups (MS-DRGs) and encompass 70% of all possible Medicare episodic expenditures. Medicare defined which services are included in the bundle for each episode and established a target price based on each provider’s historic costs for that bundle of services, minus a discount taken by Medicare. In some models, a bundled payment is made when an episode of care is initiated and is distributed by one awardee to all other providers involved in the episode. In others, providers continue to receive fee-for-service payments and Medicare reconciles these payments against the target spending amount following conclusion of the episode of care. In these retrospective reconciliation models, providers with spending below the target for an episode receive the difference from Medicare, while providers with spending above the target must pay the difference to Medicare. All models include adjustments for how sick each patient was or is expected to be. As of August 2015, 360 organizations and 1,755 partner organizations are receiving bundled payments across the four models, and Medicare continues to enroll more applicants and study initial outcomes.
In April 2016, Medicare will launch another bundled payment project, the Comprehensive Care for Joint Replacement (CCJR) model. This model will bundle Medicare payments for hip and knee replacements, which are among the most common surgeries that Medicare beneficiaries receive. In 2013, these surgeries accounted for 400,000 inpatient procedures and more than $7 billion in spending on hospital costs alone. This model is similar in many ways to BPCI, with one notable exception—participation is mandatory for hospitals located in one of 67 randomly selected Metropolitan Statistical Areas (MSAs). The bundle will include care within the hospital and for 90 days following discharge, for all hip and knee replacements. Medicare will establish a target price using a blend of hospital-specific and regional historical fee-for-service spending, minus a discount to Medicare. The amount of the discount is dependent upon quality scores, and hospitals may earn back a portion of the discount by providing Medicare with patient-reported outcomes information. Payments are reconciled retrospectively—providers bill for and receive fee-for-service payments for an entire model year, and if a hospital spends below its target and achieves quality thresholds, they receive the difference from Medicare, up to a cap. If hospital spending is above the threshold, the hospital must pay the difference to Medicare, subject to a phased-in schedule.
Planning for the PROMETHEUS (Provider payment Reform for Outcomes, Margins, Evidence, Transparency Hassle-reduction, Excellence, Understandability and Sustainability) payment model began in 2007, and it is used today by health plans and large self-funded employers. This model bundles payments around “a comprehensive episode of medical care that covers all patients services related to a single illness or condition” in an effort to encourage provider collaboration for effective, efficient care. Francois de Brantes, executive director of the Health Care Incentives Improvement Institute, which houses the PROMETHEUS model, says the model’s goal is not to save payers money, per se, but to reduce the rate of medical cost inflation over time. Commonly accepted clinical guidelines and expert opinions are used to define covered services across all providers needed to treat a condition from start to finish. The prices of these services are combined to establish an Evidence-Informed Case Rate (ECR), around which payers and providers may negotiate payments for an episode of care, adjusted for patient severity and complexity. ECRs have been established for more than 90 episodes of care and are available for public use.
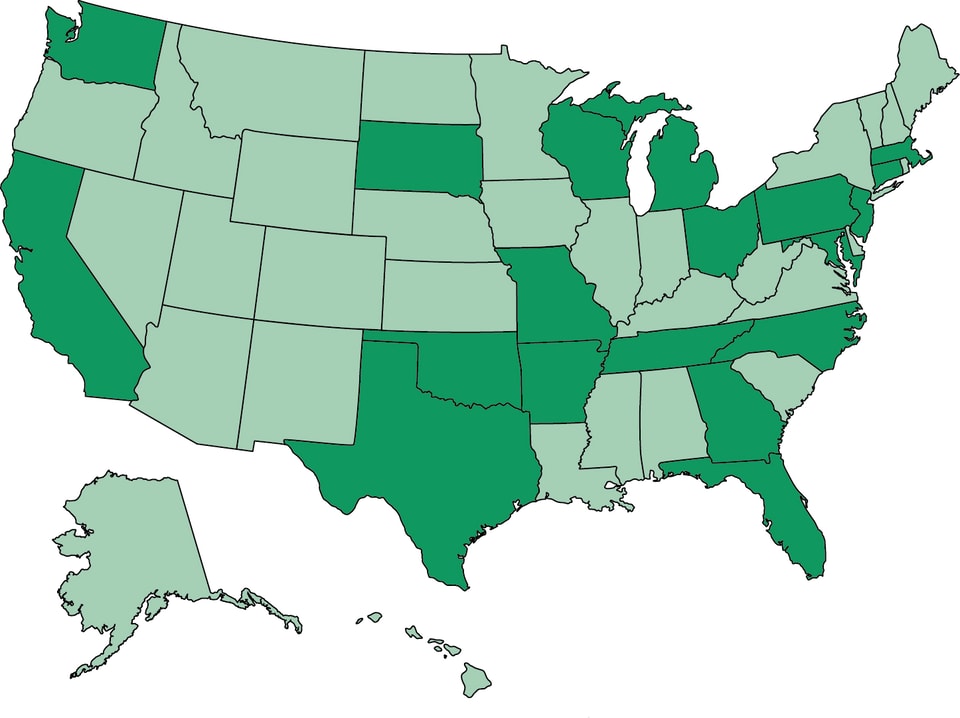
California, Maryland, Missouri, Pennsylvania, and Washington
Self-funded employers are also utilizing bundled payments to lower health care costs and improve care quality. The Employers Centers of Excellence Network, a project of the Pacific Business Group on Health, launched bundled payments in 2014 for hip and knee replacements conducted at 4 centers of excellence across the country: Virginia Mason Medical Center in Seattle, Washington; Mercy Hospital in Springfield, Missouri; Kaiser Permanente Irvine Medical Center in Irvine, California; and Johns Hopkins Bayview Medical Center in Baltimore, Maryland. Employees covered by health plans of the participating employers, including Walmart, Lowe’s, McKesson, and JetBlue, may choose to receive care from a center of excellence or from a local provider. Care from a center of excellence is provided at no cost to the patient, and the employers also cover travel, lodging, and living expenses for the patient and one caregiver. A patient advocate helps to coordinate surgery scheduling, insurance claims, and transition back to the patient’s home physician. In 2015, the Network expanded the program to include spine surgeries provided at Virginia Mason, Mercy Hospital, and Geisinger Medical Center in Danville, Pennsylvania. Beginning in April 2016, Virginia Mason will also be participating in Medicare’s Comprehensive Care for Joint Replacement model, as Seattle is one of the areas in which participation will be mandatory for hospitals.
Florida, Georgia, Ohio, Tennessee, and Texas
Five medical groups from across the country participated in a pilot program with UnitedHealthcare using an episode, or bundled, payment model to treat patients with breast, colon, or lung cancer. The unique reimbursement model for medical oncologists makes cancer care are good target for bundled payments. Physicians buy chemotherapy drugs from manufacturers at wholesale prices, then “sell” them to payers at retail prices, for a profit. This system encourages use of higher cost drugs and discourages use of lower cost generics. In the pilot program, each oncology group selected the treatment regimen it believed best for 19 clinical episodes in breast, colon, and lung cancer, Groups were allowed to change the selected regimen at any time, but the episode payment was not adjusted to reflect changes. The groups received an episode payment at a patient’s initial visit and were paid the average sales price for drugs administered during treatment. All other services were billed and paid on a traditional fee-for-service basis. Physicians also provided clinical data on each patient to UnitedHealthcare and all five groups met each year to review cost and quality data. Over 3 years, treatment for 810 patients was paid under the episode pilot, resulting in medical cost savings of more than $33 million relative to predicted fee for service costs, a 34% reduction. Savings were attributed to reduced radiation treatment, imaging, and hospitalizations. Unexpectedly, chemotherapy drug costs increased by nearly $13.5 million relative to predicted costs, a 179% increase. Of the many quality measures monitored, none showed early signs that quality varied as a result of patient enrollment in the pilot program. Participating medical groups were: Advanced Medical Specialties in Miami, Florida; the Center for Cancer and Blood Disorders in Fort Worth, Texas; Dayton Physicians in Dayton, Ohio; Northwest Georgia Oncology in Atlanta, Georgia; and West Clinic in Memphis, Tennessee.
Arkansas
The state of Arkansas and its Medicaid program have partnered with the two dominant commercial insurers to use common bundle definitions and quality measures that started in July 2012. Across the state, physicians and hospitals utilize common, bundled payment methodologies for over a dozen episodes of care, including key cost driving conditions like total joint replacements, congestive heart failure, late pregnancies, and asthma treatment. For each episode of care, a “principal accountable provider” is assigned, and providers responsible for particularly efficient and high-quality episodes of care share in savings. This work will help prepare providers in Crittenden, Benton, and Garland counties for the bundled payments they will receive for hip and knee replacements starting in April 2016 under Medicare’s Comprehensive Care for Joint Replacement model. In addition, some hospitals in the state are also participating in Medicare’s Bundled Payment for Care Improvement Initiative, which has similar incentives, and Medicare has given the state a grant through its State Innovation Model to further streamline the state and federal bundled payment models to minimize burden on providers. Though studies of private and public payer savings are still underway, the business case for alignment is clear to insurance executives in the state.
California
Hoag Orthopedic Institute is the largest volume orthopedic hospital/provider in California and was an early adopter of bundled payments. Hoag currently has bundled payment contracts with 3 commercial payers for joint replacement procedures and has initiated more than 250 bundled payment episodes. Harvard Business Review described Hoag’s success in capturing “the value created by cost-effectively delivering superior patient outcomes,” and outlined Hoag’s three keys to success. First, Hoag measures and tracks costs and outcomes for every patient, and uses additional analytics to identify process improvement opportunities. Second, Hoag proactively manages patients, such as by setting discharge expectations with patients before their procedure occurs, to capitalize on savings that may be gained by discharging patients to home health, where appropriate, rather than to a skilled nursing facility. Finally, physician-hospital alignment is critical to the success of a bundled payment effort and here, Hoag has an advantage, as physicians own 49% of the institute.
Connecticut
In 2012, the Connecticut Joint Replacement Institute at St. Francis Hospital initiated a bundled payment program with ConnectiCare, a local insurer, and a local anesthesiology group covering knee and hip replacements. A key driver of the Institute’s confidence in moving into bundled payments is a joint-replacement registry, which includes data on thousands of patients and facilitates evaluation of existing clinical protocols and how outcomes might be improved. The data available from the registry also allows for continuous improvement, delivering timely feedback on the results of care redesign activities.
Massachusetts
Bundled payments aren’t just for adults. UMass Medical School and MassHealth, the state’s Medicaid program, are partnering on a bundled payment for pediatric asthma treatment. Called the Children’s High-Risk Asthma Bundled Payment demonstration, the program’s focus is on children ages 2-18 whose asthma is likely to lead to an emergency room visit. In phase 1 of the demonstration, participating providers will receive a $50 per member per month payment to support activities not typically reimbursed by Medicaid, such as environmental home assessments conducted by community health workers or items to reduce household asthma triggers, such as vacuum filters or mattress covers. Phase 2 will involve a comprehensive bundled payment to fund traditionally-covered medical services as well as the items and services covered under phase 1. The demonstration will be limited to 200 patients.
Michigan
In the late 1980s, an orthopedic surgeon in East Lansing, Michigan, partnered with his local hospital and HMO to develop a bundled payment program for shoulder and knee arthroscopic surgery. At that time, arthroscopic surgery, which is less invasive than other surgical techniques, was not widely utilized in Michigan, and Dr. Lanny Johnson saw a potential savings, and profit, opportunity for this treatment, which was associated with faster recovery and lower hospital costs. The bundle included unlimited office visits for patients and in-office imaging, as well as all hospital charges for the surgery and all follow-up care for two years, include re-operation, if necessary. For 111 patients studied, health plan spending dropped by 39%, while hospital revenue increased by 14% and surgeon revenue increased by 82%. Quality measures were not reported.
New Jersey
Horizon Blue Cross Blue Shield of New Jersey is implementing a number of bundled payment programs across the state. The health plan now has what it calls “episode of care programs” for a range of care episodes, including pregnancy and delivery, colonoscopy, and breast cancer, using algorithms from the PROMETHEUS project. 190 physicians participate in the pregnancy and delivery bundled payment program, which covers all care during pregnancy, delivery, and post-delivery recovery and includes a shared savings opportunity if physicians meet established goals. The pregnancy and delivery bundled payment program has already achieved savings. The colonoscopy bundle is similar, with payment covering all related pre- and post-procedure services and a shared savings opportunity. The breast cancer episode of care program is a partnership with more than 100 physicians at Regional Cancer Care Associates. The program utilizes a real-time data platform that categorizes each patient’s cancer by molecular subtype, permitting a high level of treatment customization. Participating physicians are eligible for shared savings if they meet quality and efficiency goals. Horizon also utilizes bundled payments for major joint replacement, knee arthroscopy, heart failure, and coronary artery bypass graft. By expanding bundled payments to cover additional episodes of care, Horizon has moved from paying for less than 100 bundles in 2010 to more than 8,000 in 2014.
North Carolina
In 2011, Blue Cross Blue Shield of North Carolina initiated a pilot program with CaroMont Health to bundle payments for knee replacements, using a bundle definition based on the PROMETHEUS model. The bundled encompassed care provided 30 days prior to surgery, the surgery and hospitalization, and 180 days of follow-up care following discharge. The one-year program resulted in average savings of 8-10% per episode. Since this pilot program, Blue Cross Blue Shield continues to partner with additional providers in bundled payment arrangements. A bundled payment arrangement with Triangle Orthopedic Associates resulted in average cost savings of more than 22% per episode, outcomes measures above national benchmarks, potentially avoidable complication rates below the state average, and patient satisfaction scores at 97%.
Oklahoma
Hillcrest Medical Center in Tulsa, Oklahoma, participated in Medicare’s Acute Care Episode (ACE) demonstration project, which ended in 2012, for several orthopedic and cardiac procedures. During the 3-year demonstration, Hillcrest improved on many quality measures, such as a lower readmission rate and shorter average length of stay, and reduced the percentage of coronary artery bypass graft patients who returned to the operating room during their stay from 7% to 1%. However, Hillcrest was able to generate the most savings by reducing spending on implants. By standardizing device use and negotiating volume discounts with vendors, Hillcrest saved an average of 10% on cardiac implants, a savings of about $1 million, and 7% on orthopedic implants, a savings of about $450,000. Over the course of the demonstration, Hillcrest reduced Medicare spending by $814 per episode of care, for total savings of nearly $2.5 million. Interestingly, over the course of the demonstration, Hillcrest’s volume for these procedures increased between 25-40%, which administrators attribute to the relationships with physicians that Hillcrest developed during their participation in the demonstration. Hillcrest is taking lessons learned from participation in the ACE demonstration into its participation in Medicare’s Bundled Payments for Care Improvement initiative.
Pennsylvania
Geisinger Health System in Pennsylvania has made progress with its ProvenCare program, which began in 2006 for coronary artery bypass graft surgery. Geisinger charges a set rate for the surgery, all related services, and any care required within 90 days of the acute stay. In order to ensure every patient gets the right care, every time, the health system developed 40 best-care guidelines and required all staff to follow them. The model achieved impressive clinical outcomes, including reductions in in-hospital mortality (80%), neurologic and pulmonary complications (40% and 29%, respectively), 30-day readmissions (20%), and average length of stay (8%). In addition, both provider and payer benefited financially from the model, with hospital inpatient profit increasing an average of $1,946 per case while payer costs decreased about 5% relative to pre-ProvenCare costs at Geisinger, and 28-36% relative to payments to other providers. Geisinger has expanded ProvenCare to encompass 17 “service modules.”
South Dakota
Since 2011, the South Dakota State Employee Benefits Program and Black Hills Surgical Hospital have partnered to offer bundled payments on certain outpatient back procedures. The bundle includes facility fees, physician, anesthesia, and surgery charges, as well as some, limited follow-up care. Employees pay $500 for the entire bundle, compared to $1,400-$1,600 for similar procedures offered elsewhere on a non-bundled basis.
Texas
In 1984, physicians from the Texas Heart Institute developed a bundled payment for cardiovascular surgery that included all physician and hospital charges. The bundled payment option was first offered to non-Medicare patients via contracts with self-insured companies, health plans, and unions. In 1985, the bundled payment price for coronary artery bypass was $13,800, compared to Medicare’s average payment of $24,588. Texas Heart Institute physicians stated that in addition to lowering costs, the program increased patient access, allowed payers to better predict expenses, streamlined billing, and maintained high quality care.
Baptist Health System in San Antonio was a participant in Medicare’s Acute Care Episode (ACE) bundled payment demonstration under several cardiac and orthopedic procedures. Baptist experienced substantial start-up costs, spending more than $900,000 to prepare for bundled payments, largely in legal fees, infrastructure investments, and support personnel. For example, Baptist employed patient navigators to identify ACE-eligible patients for billing purposes and respond to their needs. The investment paid off, as Baptist was able to generate net savings to Medicare of $133 per episode for total savings of more than $655,000 over three years. Savings varied greatly across procedures, from just $1 per episode for hip and knee replacements to more than $1,000 per episode for cardiac defibrillator implantations. Baptist physicians developed a monthly report card to measure compliance with protocols and best practices, summarizing 40 quality measures across 10 domains. Each individual physician’s score was compared to aggregate cost and quality benchmarks to determine gainsharing eligibility. Baptist administrators felt the system’s ACE demonstration participation helped them strengthen relationships with independent specialists who, while initially wary of the program, ultimately worked with the hospital to improve quality and reduce costs.
Wisconsin
Meriter Hospital, located in Madison, WI, began receiving bundled payments for knee replacements in 2012, and in 2014 expanded the initiative to hip replacements as a participant in Medicare’s Bundled Payments for Care Improvement initiative. Meriter has invested staff in the project, hiring a project manager, dedicating a financial analyst to the program, and working with a consultant, and has also redesigned care to standardize supplies, equipment, and care pathways, working with both employed and non-employed physicians. But those efforts are yielding results. Since 2013, Meriter’s bundled payment programs for these two joint replacement procedures have achieved reductions in length of stay (12%), discharges to skilled nursing facilities (23%), an hospital readmissions (68%).
